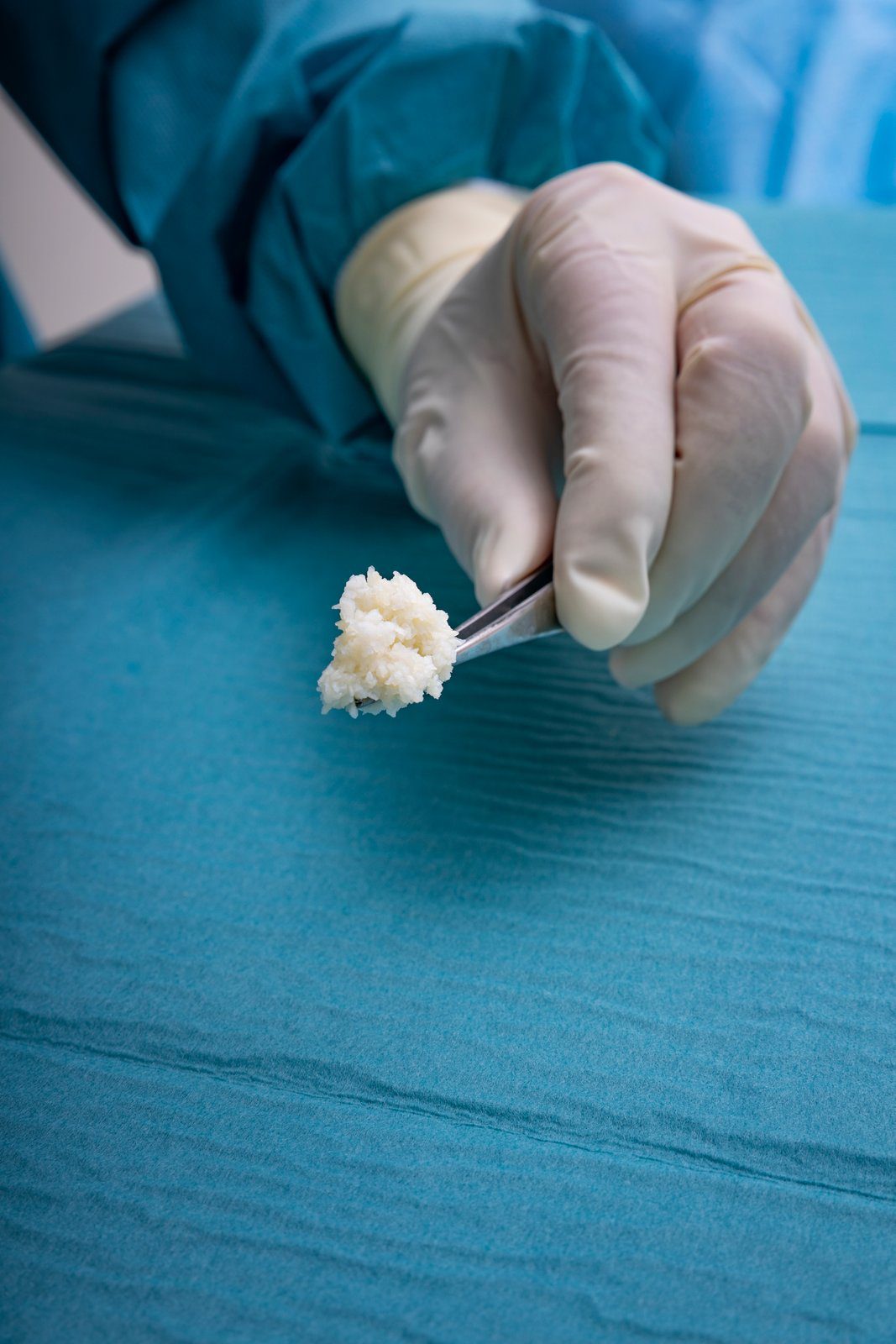
Because no known viral transfer risk exists between North-Atlantic Cod and humans, the Kerecis patented fish skin is only gently processed and retains its similarity to human skin. Compared to mammalian-based skin substitutes. Most skin substitutes products are based on tissues of human and porcine origin. These are not ideal substitutes because heavy processing is needed to eliminate the risk of disease transmission. This harsh, anti-viral treatment removes most of the material’s natural components, making it dissimilar to human skin.
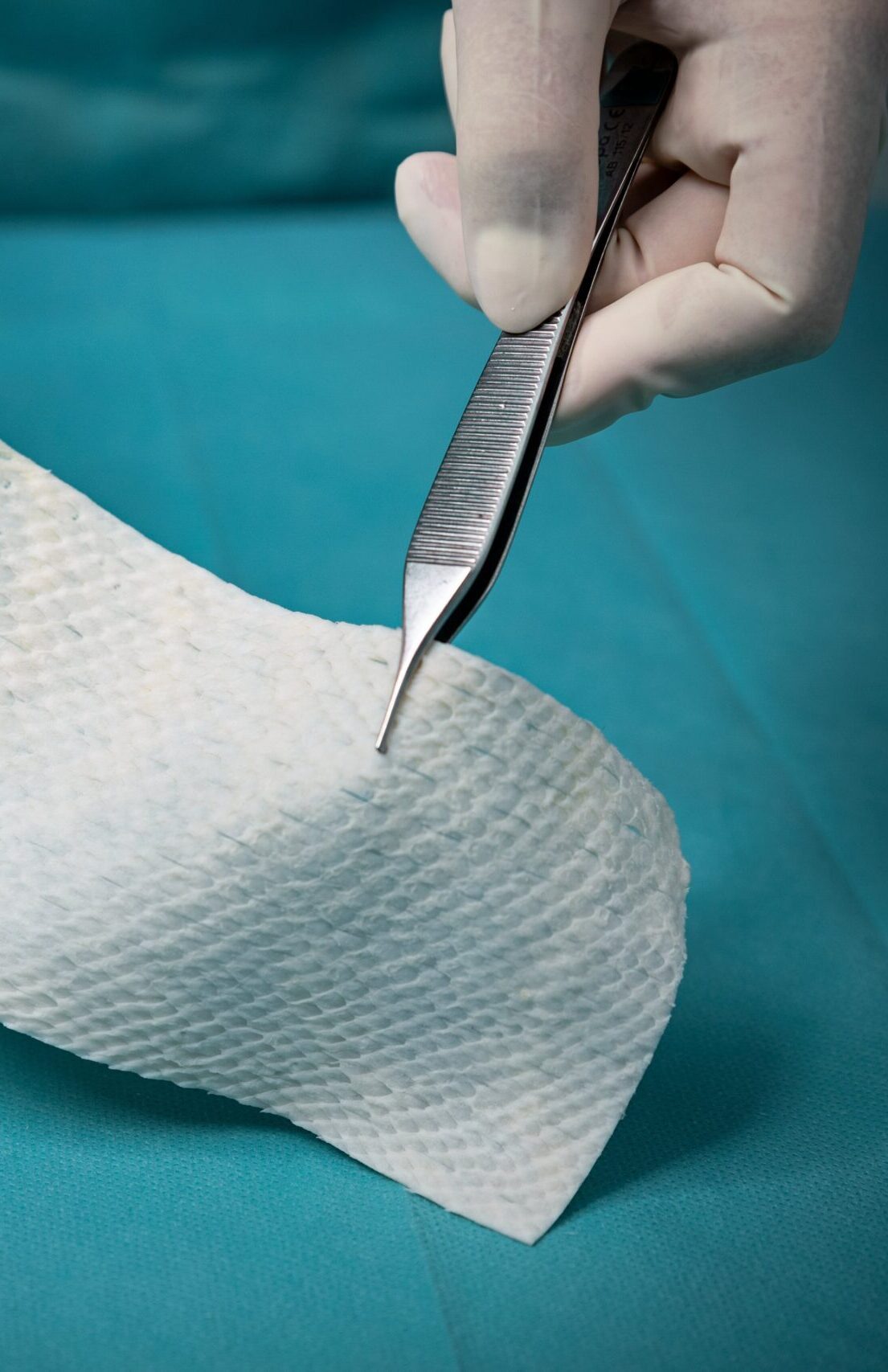
The fish are caught in the pristine waters of North Atlantic Ocean off the township of Isafjordur, on the northwest coast of Iceland. Each and every batch of raw materials is tracked to ensure product quality. The fish skin is processed using a proprietary method that preserves its structure and lipid composition.
Intact fish skin has been cleared by the FDA and European regulatory authorities for wound management. The product is undergoing registration at multiple regulatory authorities around the world.
Kerecis is pioneering the use of intact fish skin in the globally expanding cellular-therapy and regenerative-medicine markets. The unique products from the company’s patented technologies help protect the body’s own tissues and provide the ideal environment to help facilitate tissue regeneration.

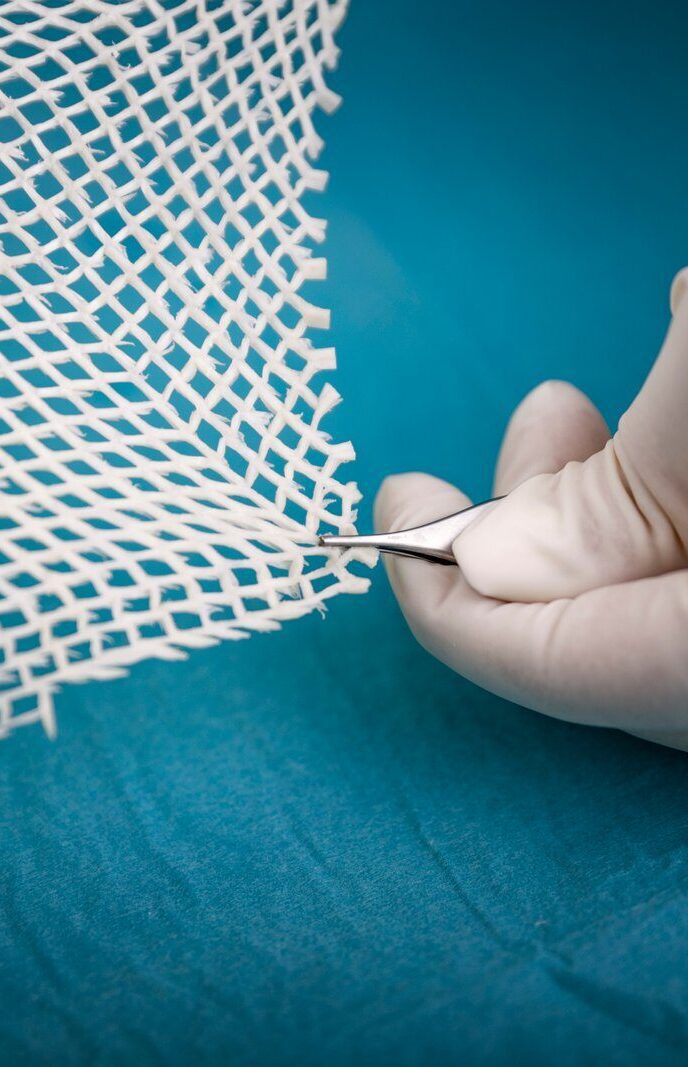
Kerecis has been awarded multiple patents protecting the core technology in the U.S. and other countries, and several more applications are pending. Kerecis is committed to building a substantial patent portfolio protecting the company´s intellectual property.